Primary Biliary Cholangitis (PBC) Clinical Trials: Current Status and Future Directions
Primary biliary cholangitis (PBC) is a chronic autoimmune disease that affects the liver’s bile ducts, leading to their inflammation, damage, and eventually scarring. Over time, this can cause liver failure, cirrhosis, and other complications. Although the exact cause of PBC is unknown, it is believed to be triggered by a combination of genetic, environmental, and immunological factors.
Clinical trials are an essential part of medical research that aim to evaluate the safety, efficacy, and tolerability of new and existing treatments for PBC. These trials involve testing experimental drugs, therapies, or procedures on human subjects under controlled conditions to determine their potential benefits and risks. Clinical trials can also help to identify biomarkers, genetic factors, and other predictors of PBC progression and response to treatment.
Key Takeaways
- PBC is a chronic autoimmune disease that affects the liver’s bile ducts, leading to inflammation, damage, and scarring.
- Clinical trials are an essential part of medical research that aim to evaluate the safety, efficacy, and tolerability of new and existing treatments for PBC.
- Clinical trials can help to identify biomarkers, genetic factors, and other predictors of PBC progression and response to treatment.
Understanding Primary Biliary Cholangitis
Primary biliary cholangitis (PBC) is a chronic, autoimmune liver disease that affects the small bile ducts within the liver. It is more common in middle-aged women, but it can also affect young women and men. The exact cause of PBC is unknown, but it is believed to be due to a combination of genetic and environmental factors.
Pathophysiology
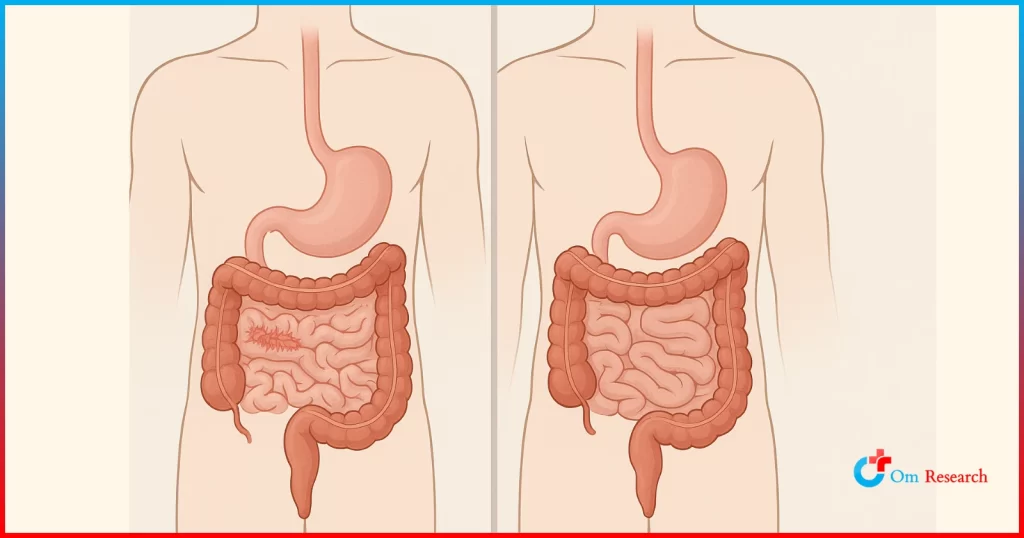
PBC is characterized by chronic inflammation and destruction of the small bile ducts within the liver. Over time, this can lead to the accumulation of bile within the liver, which can cause damage to the liver cells and eventually lead to cirrhosis and liver failure. The exact mechanism of how the immune system attacks the bile ducts is not well understood, but it is believed to be due to the presence of autoantibodies that target the cells lining the bile ducts.
Stages of PBC
PBC progresses slowly over time, and it is typically divided into four stages based on the severity of liver damage. In the early stages of PBC, patients may not experience any symptoms, and the disease may only be detected through routine blood tests. As the disease progresses, patients may experience symptoms such as fatigue, itching, and abdominal pain. In the later stages of the disease, patients may develop cirrhosis, which can lead to complications such as portal hypertension, ascites, and hepatic encephalopathy.
Overall, PBC is a complex disease that requires careful management and monitoring. While there is no cure for PBC, there are treatments available that can help slow the progression of the disease and manage symptoms. Clinical trials are ongoing to develop new treatments for PBC, and patients are encouraged to speak with their healthcare provider about participating in these trials.
Diagnosis and Monitoring
Diagnostic Criteria
Primary biliary cholangitis (PBC) is a chronic autoimmune liver disease that is characterized by the destruction of small bile ducts within the liver. The diagnosis of PBC is based on a combination of clinical, laboratory, and histological criteria. According to the American Association for the Study of Liver Diseases (AASLD) guidelines, the diagnosis of PBC requires the presence of at least two of the following three criteria:
- Elevated serum alkaline phosphatase (ALP) levels for more than six months
- Presence of anti-mitochondrial antibodies (AMA)
- Liver biopsy showing florid duct lesion consistent with PBC
It is important to note that some patients may have normal ALP levels, but still meet the diagnostic criteria based on the presence of AMA and/or liver biopsy findings. Therefore, a liver biopsy is often recommended in patients with suspected PBC, even if the ALP levels are normal.
Monitoring Progression
Once a diagnosis of PBC is established, monitoring disease progression is critical to prevent complications such as cirrhosis and liver failure. The AASLD recommends that patients with PBC undergo periodic monitoring with laboratory tests and imaging studies.
Laboratory tests should include measurement of serum ALP, bilirubin, alanine aminotransferase (ALT), aspartate aminotransferase (AST), and albumin levels. In addition, patients should be screened for the presence of other autoimmune diseases, as these are commonly associated with PBC.
Imaging studies, such as ultrasound or magnetic resonance cholangiopancreatography (MRCP), may be used to assess the severity of bile duct damage and to detect the presence of complications such as portal hypertension or liver nodules.
For patients who have progressed to advanced stages of PBC, liver transplantation may be considered as a treatment option. In these cases, close monitoring of disease progression is critical to ensure that the patient is referred for transplantation at the appropriate time.
Clinical Trials Overview
Importance of Clinical Trials
Clinical trials are an essential part of medical research that involves testing new treatments, therapies, and drugs on humans. They are designed to evaluate the safety and efficacy of new interventions, and to determine the optimal dosage, administration route, and side effects of these interventions. Clinical trials are crucial for the development of new treatments for primary biliary cholangitis (PBC), a chronic autoimmune liver disease that affects the bile ducts and can lead to cirrhosis, liver failure, and death.
Clinical trials are important for several reasons. First, they provide patients with access to cutting-edge treatments that may not be available otherwise. Second, they help researchers identify new treatments that can improve the quality of life and survival of patients with PBC. Third, they contribute to the advancement of medical knowledge and the development of new therapies for other liver diseases.
Phases of Clinical Trials
Clinical trials are typically divided into four phases, each with a specific goal and design. Phase I trials are the first step in testing new treatments in humans and are designed to evaluate the safety and tolerability of the treatment. Phase II trials are designed to evaluate the efficacy of the treatment in a small group of patients. Phase III trials are designed to confirm the efficacy and safety of the treatment in a larger group of patients. Phase IV trials are post-marketing studies that evaluate the long-term safety and efficacy of the treatment in a real-world setting.
In PBC clinical trials, the primary endpoint is often the reduction of serum alkaline phosphatase (ALP) levels, a marker of liver damage. Secondary endpoints may include improvement in liver function, quality of life, and survival. Clinical trials may also evaluate the efficacy of combination therapies, such as the combination of ursodeoxycholic acid (UDCA) and obeticholic acid (OCA), in patients with PBC.
In conclusion, clinical trials are essential for the development of new treatments for PBC and other liver diseases. They provide patients with access to cutting-edge treatments, contribute to the advancement of medical knowledge, and improve the quality of life and survival of patients with PBC.
Current and Emerging Treatments
Standard Treatment Approaches
Primary biliary cholangitis (PBC) is a chronic autoimmune disease of the liver that can progress to cirrhosis and liver failure. The current standard of care for PBC is ursodeoxycholic acid (UDCA) therapy. UDCA is a bile acid that has been shown to improve liver function and survival in patients with PBC. The recommended dose of UDCA is weight-based, and current guidelines recommend starting at a dose of 13 to 15 mg/kg, divided in 2 to 3 doses per day [1].
However, up to 40% of patients with PBC do not respond to UDCA therapy, and some patients may experience intolerable side effects [2]. In these cases, alternative treatment options are needed. The use of immunosuppressive agents, such as corticosteroids, has been investigated in PBC, but the evidence for their efficacy is limited and they are associated with significant side effects [3].
Investigational Therapies
Several investigational therapies are currently being studied in clinical trials for the treatment of PBC. These therapies target different aspects of the disease, including the immune system, bile acid metabolism, and fibrosis.
One promising investigational therapy is obeticholic acid (OCA), a modified bile acid that activates the farnesoid X receptor (FXR) and regulates bile acid metabolism. OCA has been shown to improve liver function and reduce fibrosis in patients with PBC in clinical trials [4]. Another investigational therapy is bezafibrate, a lipid-lowering drug that has been shown to improve liver function and reduce inflammation in patients with PBC [5].
Other investigational therapies being studied in clinical trials for PBC include:
- Seladelpar, a selective peroxisome proliferator-activated receptor delta (PPAR-delta) agonist that regulates lipid metabolism and inflammation [6].
- Maralixibat, an inhibitor of the apical sodium-dependent bile acid transporter (ASBT) that regulates bile acid absorption [7].
- Simtuzumab, a monoclonal antibody that targets the extracellular matrix protein lysyl oxidase-like 2 (LOXL2) and reduces fibrosis in the liver [8].
Overall, the development of new therapies for PBC is an active area of research, and several promising investigational therapies are currently being studied in clinical trials. Further research is needed to determine the safety and efficacy of these therapies in patients with PBC.
Living with Primary Biliary Cholangitis
Living with Primary Biliary Cholangitis (PBC) can be challenging, especially when dealing with its symptoms. However, there are ways to manage the disease and improve the quality of life for those affected by it.
Lifestyle and Management
One of the most important aspects of managing PBC is maintaining a healthy lifestyle. This includes:
- Eating a balanced diet: A healthy diet can help manage PBC symptoms and prevent complications. Patients should avoid alcohol, fatty foods, and excessive amounts of salt and sugar.
- Exercising regularly: Regular exercise can help improve energy levels, manage weight, and reduce stress.
- Getting enough rest: Fatigue is a common symptom of PBC. Patients should prioritize getting enough rest and sleep to manage their symptoms.
- Taking medications as prescribed: Medications can help manage PBC symptoms and prevent complications. Patients should take their medications as prescribed and inform their doctor of any side effects.
Patient Support and Resources
Living with PBC can be challenging, but patients do not have to face it alone. There are many resources available to help patients manage their symptoms and improve their quality of life.
- Support groups: Joining a support group can help patients connect with others who are going through similar experiences and share tips and advice.
- Patient education: Many organizations offer resources and educational materials to help patients better understand PBC and manage their symptoms.
- Clinical trials: Participating in clinical trials can give patients access to new treatments and help advance research on PBC.
By following a healthy lifestyle and utilizing available resources, patients with PBC can manage their symptoms and improve their quality of life.
Frequently Asked Questions
How can I enroll in a clinical trial for E. Coli infection at Om Research?
A: visit our website or contact our team for more information. We welcome individuals who meet the trial criteria to contribute to this important research.
What are the latest advancements in the treatment of Primary Biliary Cholangitis?
Recent studies have shown that obeticholic acid (OCA) has been effective in the treatment of PBC. OCA is a synthetic bile acid that has been shown to improve liver function and reduce the progression of liver fibrosis. Another promising treatment is bezafibrate, which has been shown to improve liver function and reduce the levels of liver enzymes.
Which medications have been approved by the FDA for the management of PBC?
The FDA has approved several medications for the treatment of PBC, including ursodeoxycholic acid (UDCA), obeticholic acid (OCA), and rifampin. UDCA is the most commonly prescribed medication and has been shown to improve liver function and reduce the progression of liver fibrosis.
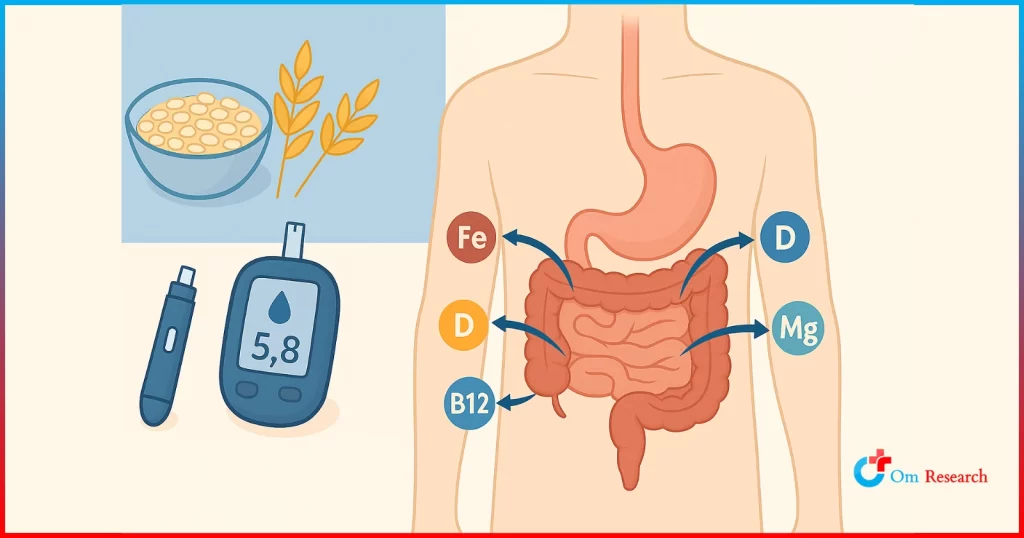
What dietary considerations should be taken into account for patients with PBC?
Patients with PBC should follow a healthy, balanced diet that is low in fat and high in fiber. It is also important to avoid alcohol and limit the intake of processed foods and saturated fats. Patients should consult with their healthcare provider or a registered dietitian for personalized dietary recommendations.
Can Primary Biliary Cholangitis be considered a disability for insurance purposes?
PBC can be considered a disability for insurance purposes if it significantly impacts a patient’s ability to work or perform daily activities. Patients with PBC may be eligible for disability benefits if they are unable to work due to the symptoms of the disease.
Sources
[1] Current and Emerging Treatment Options for Primary Biliary Cholangitis
[2] Management of Primary Biliary Cholangitis: Current Treatment and Future Directions
[3] Emerging drugs for the treatment of Primary Biliary Cholangitis