Irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) are two gastrointestinal disorders that can cause significant discomfort and disruption in a person’s life.
While they share the same symptoms, they are distinct conditions with different underlying causes and treatment options.
IBS is a functional disorder, meaning that there is no structural abnormality in the digestive tract. It is characterized by symptoms such as abdominal pain, bloating, and irregular bowel movements.
However, IBD is an inflammatory condition that can damage the digestive tract.
The two main types of IBD are Crohn’s disease and ulcerative colitis, both of which can cause symptoms such as diarrhea, abdominal pain, and rectal bleeding.
Understanding the differences between IBS and IBD is important for accurate diagnosis and treatment.
While there is currently no cure for either condition, there are various treatment options available that can help manage symptoms and improve quality of life.
Understanding Irritable Bowel Syndrome
What Is Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) is a common gastrointestinal disorder that affects the large intestine. It is a chronic condition that causes a group of symptoms, including abdominal pain, bloating, and changes in bowel movements. IBS is a functional disorder, meaning that there is no structural abnormality in the gut, but it affects the way the gut works.
Symptoms of Irritable Bowel Syndrome
The symptoms of IBS can vary from person to person, but the most common ones include:
- Abdominal pain or cramping
- Bloating and gas
- Diarrhea or constipation, or both
- Mucus in the stool
- Feeling of incomplete bowel movement
The symptoms can be mild to severe and can come and go over time. They can be triggered by certain foods, stress, hormonal changes, and other factors.
Causes of Irritable Bowel Syndrome
The exact cause of IBS is unknown, but several factors may contribute to its development. These include:
- Abnormalities in the gut-brain axis, which controls the gut’s motility and sensitivity
- Changes in the gut microbiome, which is the collection of microorganisms that live in the gut
- Food sensitivities or allergies
- Stress and anxiety
- Hormonal changes
Some people may have a genetic predisposition to IBS, but more research is needed to understand the role of genetics in the development of this condition.
In conclusion, IBS is a common gastrointestinal disorder that affects the large intestine. It is a chronic condition that causes a group of symptoms, including abdominal pain, bloating, and changes in bowel movements.
The exact cause of IBS is unknown, but several factors may contribute to its development.
Understanding Inflammatory Bowel Disease
What Is Inflammatory Bowel Disease
Inflammatory Bowel Disease (IBD) is a chronic inflammatory disorder that affects the digestive tract. It is a term used to describe two conditions: Crohn’s disease and Ulcerative Colitis.
Crohn’s disease can affect any part of the digestive tract, while Ulcerative Colitis affects only the colon and rectum.
IBD is a chronic condition that requires lifelong management.
Symptoms of Inflammatory Bowel Disease
The symptoms of IBD can vary from person to person and depend on the severity of the disease.
Common symptoms of IBD include:
- Diarrhea
- Abdominal pain
- Cramping
- Rectal bleeding
- Weight loss
- Fatigue
In severe cases, IBD can lead to complications such as bowel obstruction, abscesses, and fistulas.
Causes of Inflammatory Bowel Disease
The exact cause of IBD is unknown, but it is believed to be the result of a combination of genetic, environmental, and immune system factors.
Research suggests that IBD may be caused by an abnormal immune response to a virus or bacteria in the digestive tract.
Other factors that may contribute to the development of IBD include smoking, stress, and certain medications.
In conclusion, IBD is a chronic inflammatory disorder affecting the digestive tract and is characterized by symptoms like diarrhea, abdominal pain, cramping, rectal bleeding, weight loss, and fatigue.
The exact cause of IBD is unknown, but it is believed to be the result of a combination of genetic, environmental, and immune system factors.
Comparing IBS and IBD
IBS vs. IBD
Irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) are two gastrointestinal disorders that are often confused with each other. However, there are some key differences between the two.
IBS is a functional disorder that affects the large intestine. It is characterized by symptoms such as abdominal pain, bloating, and changes in bowel movements.
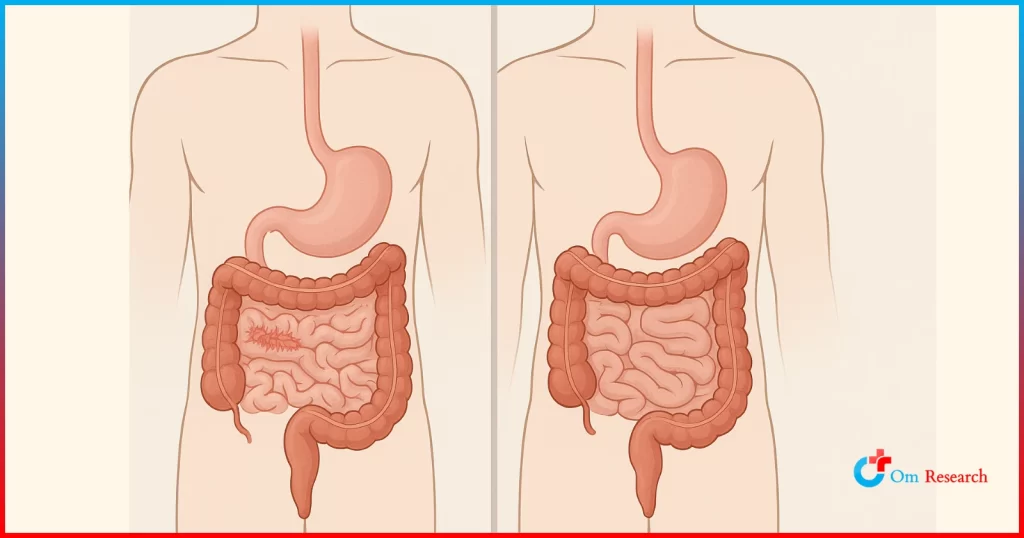
Unlike IBD, IBS does not cause inflammation or damage to the intestinal lining.
IBD, on the other hand, is a group of chronic inflammatory disorders that affect the digestive tract.
The two main types of IBD are Crohn’s disease and ulcerative colitis. Both conditions cause inflammation and damage to the intestinal lining, which can lead to a range of symptoms such as abdominal pain, diarrhea, and rectal bleeding.
Irritable Bowel Syndrome vs Crohn’s Disease
Crohn’s disease is a type of IBD that can affect any part of the digestive tract, from the mouth to the anus.
The inflammation caused by Crohn’s disease can be patchy, meaning that there may be healthy sections of intestine between areas of inflammation. This can make it difficult to diagnose and treat.
In contrast, IBS is limited to the large intestine and does not cause inflammation.
While Crohn’s disease can cause symptoms such as abdominal pain, diarrhea, and weight loss, IBS typically causes less severe symptoms such as bloating and changes in bowel movements.
Ulcerative Colitis vs irritable bowel syndrome
Ulcerative colitis is another type of IBD that affects the large intestine and rectum. Unlike Crohn’s disease, which can affect any part of the digestive tract, ulcerative colitis is limited to the colon and rectum.
Like Crohn’s disease, ulcerative colitis causes inflammation and damage to the intestinal lining.
This can lead to symptoms such as abdominal pain, diarrhea, and rectal bleeding.
In contrast, IBS does not cause inflammation and typically causes less severe symptoms such as bloating and changes in bowel movements.
Overall, while IBS and IBD share some similarities in terms of symptoms, they are two distinct conditions with different underlying causes and treatment approaches.
It is important to consult a healthcare provider to determine the appropriate diagnosis and treatment plan.
Diagnosis and Treatment
Diagnosing IBS and IBD
Diagnosing IBS and IBD can be challenging as the symptoms of both conditions can be similar.
However, there are several diagnostic tests available that can help distinguish between the two conditions.
For IBS, the diagnosis is typically made based on the patient’s symptoms and medical history.
According to a review published in JAMA, there are no specific diagnostic tests for IBS, but tests may be performed to rule out other conditions that may have similar symptoms, such as celiac disease or inflammatory bowel disease.
However, diagnosing IBD usually involves a combination of tests, including blood tests, stool tests, endoscopy, and imaging tests.
Endoscopy is considered the gold standard for diagnosing IBD.
Treatment Options for IBS
Treatment for IBS typically involves a combination of lifestyle changes and medication. According to a review published in Discovery Medicine, dietary modifications, such as avoiding certain foods that may trigger symptoms, can be effective in managing IBS symptoms.
In addition, medications such as antispasmodics, laxatives, and antidepressants may also be prescribed to alleviate symptoms. According to a review published in the American Journal of Gastroenterology, probiotics may also be effective in reducing IBS symptoms.
Treatment Options for IBD
Treatment for IBD varies depending on the severity of the condition. Mild cases may be treated with anti-inflammatory drugs, such as 5-aminosalicylates. Moderate to severe cases may require immunosuppressive drugs, such as corticosteroids or biologics.
According to a review published in the Journal of Crohn’s and Colitis, surgery may also be necessary in some cases, particularly in patients with complications such as bowel obstruction or perforation.
Overall, early diagnosis and treatment of both IBS and IBD can help manage symptoms and improve quality of life for patients.
Living with IBS and IBD
Living with irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) can be challenging, but there are ways to manage the symptoms and improve quality of life. Here are some considerations for those living with IBS and IBD.
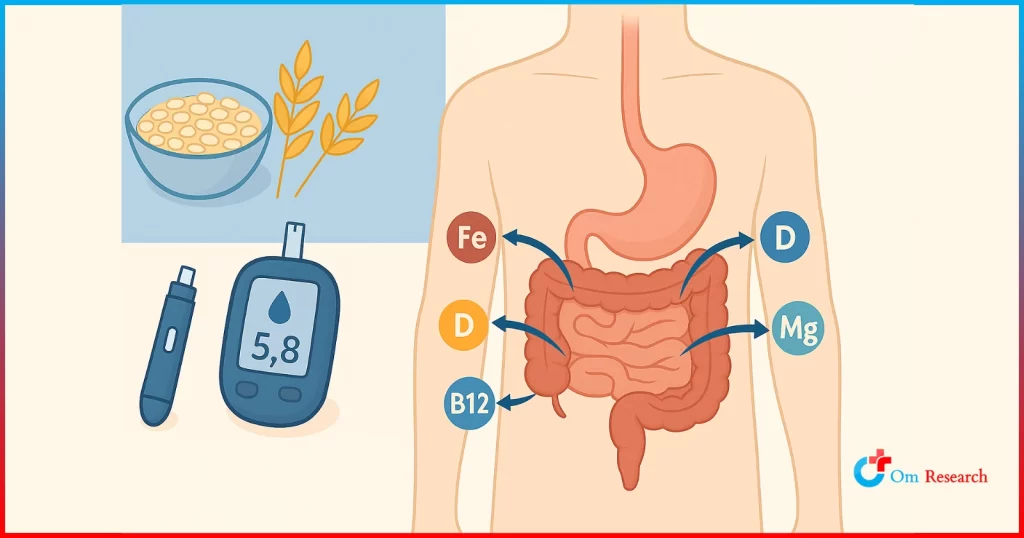
Dietary Considerations
Diet plays an important role in managing symptoms of IBS and IBD. People with IBS may benefit from avoiding certain foods that trigger symptoms such as bloating, gas, and diarrhea. Some common triggers include high-fat foods, caffeine, alcohol, and spicy foods. On the other hand, people with IBD may need to follow a low-fiber diet during flare-ups to reduce inflammation and improve symptoms. It is important to work with a healthcare provider or a registered dietitian to develop an individualized diet plan that meets nutritional needs and helps manage symptoms.
Lifestyle Adjustments
Making lifestyle adjustments can also help manage symptoms of IBS and IBD. For example, stress can trigger symptoms in both conditions, so it is important to find ways to manage stress such as practicing relaxation techniques, getting enough sleep, and engaging in regular exercise. Additionally, people with IBD may benefit from avoiding nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin and ibuprofen, as these can worsen inflammation in the gut.
Further Resources
Diagnosis and Treatment of Irritable Bowel Syndrome – Nicole C Suares – Discovery Medicine
Role of endoscopy in inflammatory bowel disease – PMC (nih.gov)
Inflammatory bowel disease (IBD) – Symptoms and causes – Mayo Clinic
What is inflammatory bowel disease (IBD)? | IBD (cdc.gov)
Symptoms & Causes of Irritable Bowel Syndrome – NIDDK (nih.gov)
Irritable bowel syndrome – Symptoms and causes – Mayo Clinic
Frequently Asked Questions
What are the distinguishing symptoms between IBS and IBD?
Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD) share some common symptoms such as abdominal pain, diarrhea, and fatigue. However, IBD is associated with more severe symptoms such as rectal bleeding, weight loss, and fever. In contrast, IBS is characterized by a change in bowel habits, bloating, and discomfort that is often relieved after a bowel movement.
How can IBD be differentiated from Crohn’s disease and ulcerative colitis?
Crohn’s disease and ulcerative colitis are the two main types of IBD. Crohn’s disease can affect any part of the digestive tract, from the mouth to the anus, while ulcerative colitis only affects the colon and rectum. Additionally, Crohn’s disease can cause inflammation that penetrates the entire thickness of the intestinal wall, while ulcerative colitis only affects the innermost lining of the colon.
What are common triggers for IBS flare-ups?
IBS flare-ups can be triggered by a variety of factors, including stress, certain foods, hormonal changes, and medications. Common trigger foods include fatty or fried foods, dairy products, caffeine, alcohol, and spicy foods.
Is it possible to suffer from both IBS and IBD simultaneously?
Yes, it is possible to have both IBS and IBD simultaneously. In fact, studies have shown that up to 30% of patients with IBD may also have symptoms of IBS.
How is IBD diagnosed in contrast to IBS?
IBD is typically diagnosed through a combination of medical history, physical examination, blood tests, and imaging studies such as colonoscopy or CT scan. In contrast, IBS is diagnosed based on the presence of characteristic symptoms and the absence of any underlying structural or biochemical abnormalities.
What dietary changes can alleviate symptoms of IBS?
Dietary changes that may alleviate symptoms of IBS include increasing fiber intake, avoiding trigger foods, and eating smaller, more frequent meals. Additionally, some studies suggest that probiotics may be helpful in reducing symptoms of IBS. It is important to work with a healthcare provider or registered dietitian to develop an individualized dietary plan.