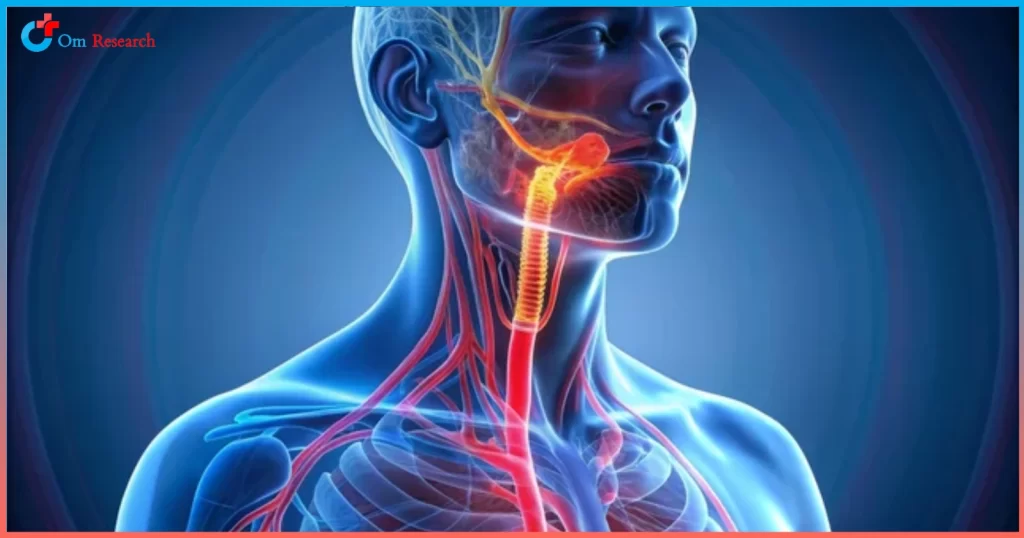
Barrett’s esophagus is a medical condition that occurs when the lining of the esophagus changes due to prolonged exposure to stomach acid.
This condition is often associated with chronic acid reflux, also known as GERD (Gastroesophageal Reflux Disease), although it doesn’t always cause noticeable symptoms.
But Barrett’s esophagus is a serious condition that can progress to esophageal cancer if left untreated.
In this blog, we’ll explore everything you need to know about Barrett’s esophagus, including causes, symptoms, diagnosis, and management and protection.
What is Barrett’s Esophagus?
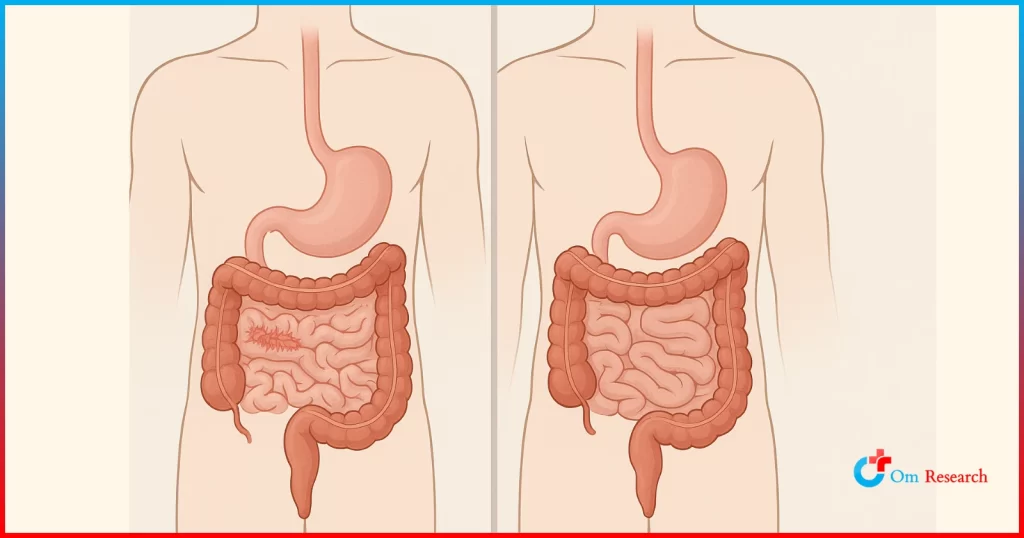
Barrett’s esophagus is when the lining of the esophagus is replaced by tissue similar to the inner lining. This process is called intestinal metaplasia.
It usually occurs because of acid reflux or prolonged acid reflux. When stomach acid repeatedly irritates the esophagus. It may cause cell damage.
Essential facts to know:
Barrett’s esophagus itself does not cause symptoms. Symptoms are often caused by acid reflux, such as heartburn or recurrent heartburn.
About 10-15% of people with chronic GERD have Barrett’s esophagus.
This condition increases your risk of a type of esophageal cancer called esophageal adenocarcinoma. However, this risk is still relatively low.
Understanding this condition is essential for early detection and efficient management.
Risk Factors and Subtle Sign
Barrett’s esophagus often develops without apparent symptoms. But there are a number of factors that can increase your chances of developing the condition. Knowing these things can help identify people who may be at risk.
Common risk factors:
Chronic GERD: Chronic GERD is the most critical risk factor.
Age: Most cases occur in people over 50 years of age.
Gender: Men are more likely than women to develop Barrett’s esophagus.
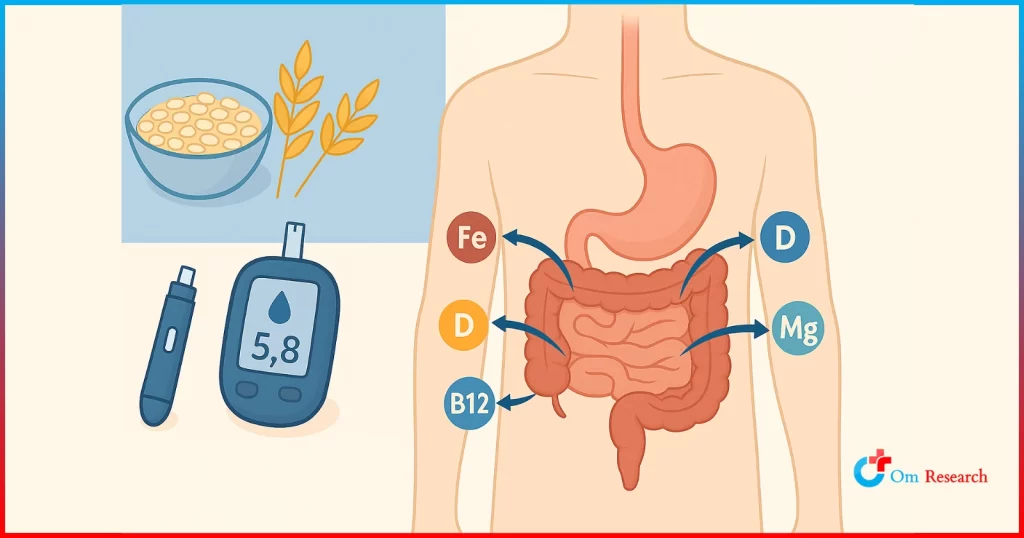
Obesity: Excess body weight increases intra-abdominal pressure and reduces contractions.
Smoking: Tobacco irritates the esophagus and increases reflux.
Family history: Genetic predisposition may play a role.
Signs to watch for:
Although Barrett’s esophagus itself is asymptomatic, symptoms of acid reflux, such as heartburn, difficulty swallowing, and constant coughing, should be encouraged to receive treatment. Recognizing symptoms of GERD can lead to intervention at the root cause of an underlying condition, such as Barrett’s esophagus.
Diagnosing Barrett’s Esophagus
Accurate diagnosis is critical to managing Barrett’s esophagus and reducing the risk of complications. If you have chronic acid reflux or are in a high-risk group, your doctor may recommend testing to confirm this condition.
Diagnosis method:
Upper endoscopy: A flexible tube with a camera is inserted into the esophagus to look at changes in the lining.
Biopsy: During endoscopy, A small sample of esophageal tissue will be taken for laboratory analysis to identify intestinal metaplasia.
Surveillance program: Patients diagnosed with Barrett’s esophagus can undergo regular endoscopy to monitor for signs of pathology (abnormal metastatic cancer cells).
Early detection is considered the key to preventing the progression of esophageal cancer. If you are at risk, don’t wait to get a medical evaluation.
How is Barrett’s Esophagus Treated?
Treatment focuses on managing GERD, preventing further esophageal damage and tracking cancer changes. The method depends on the severity of the symptoms.
Lifestyle changes:
Minor changes to your daily routine can significantly reduce acid reflux symptoms and protect your esophagus:
- Avoid stimulating foods such as caffeine, alcohol, spicy foods, and citrus.
- Eat a light meal and avoid to bed immediately after eating.
- Raise the head of your bed to reduce nighttime acid reflux.
- Maintain a healthy weight to reduce intra-abdominal pressure.
Medical intervention:
Medications: Proton pump inhibitors (PPIs) and H2 blockers can reduce stomach acid production and reduce symptoms.
Endoscopic therapy: Procedures such as radiofrequency ablation or endoscopic surgery. It can remove damaged cells or prevent the progression of dysplasia.
Surgery: Surgery to prevent acid reflux may be recommended. Fundoplication or esophageal surgery in severe cases
Collaborating with your healthcare provider to create a customized treatment plan for effective management is essential.
Prevention and Long-Term Outlook
Although not all cases of Barrett’s esophagus can be prevented, taking a proactive approach can reduce risk and significantly improve prognosis.
Prevention tips:
- Manage symptoms of GERD with a combination of medication and lifestyle changes.
- Quit smoking to reduce irritation to the esophagus and improve overall health.
- Limit alcohol intake. It can make acid reflux worse and damage your esophagus.
- Eat a balanced diet rich in fruits, vegetables, and whole grains to maintain a healthy weight.
If you have GERD or other risk factors, make regular health check appointments.
Long-term view:
Most people with Barrett’s esophagus live everyday life with proper management. Although this condition increases the risk of esophageal cancer, regular monitoring and timely treatment can significantly reduce this risk. Patients diagnosed with Barrett’s esophagus should work closely with their healthcare provider to develop a long-term care plan.
Conclusion
Barrett’s esophagus is a condition that must be treated, especially for people with chronic acid reflux disease.
By understanding the risk factors, the importance of early diagnosis, and implementing effective treatment strategies, you will be able to manage your condition and prevent complications.
If you have persistent acid reflux symptoms or other risk factors, consult your doctor immediately for evaluation.