The relationship between mental health and physical well-being has never been more evident than in the intricate bond between the gut and the brain. For individuals living with irritable bowel syndrome (IBS), this connection isn’t just theoretical—it’s a daily reality. Stress, a universal yet deeply personal experience, can act as both a trigger and a multiplier of IBS symptoms, creating a cycle that impacts not only digestion but also emotional health. Here’s how the gut-brain axis shapes IBS—and why addressing stress is often key to breaking the cycle.
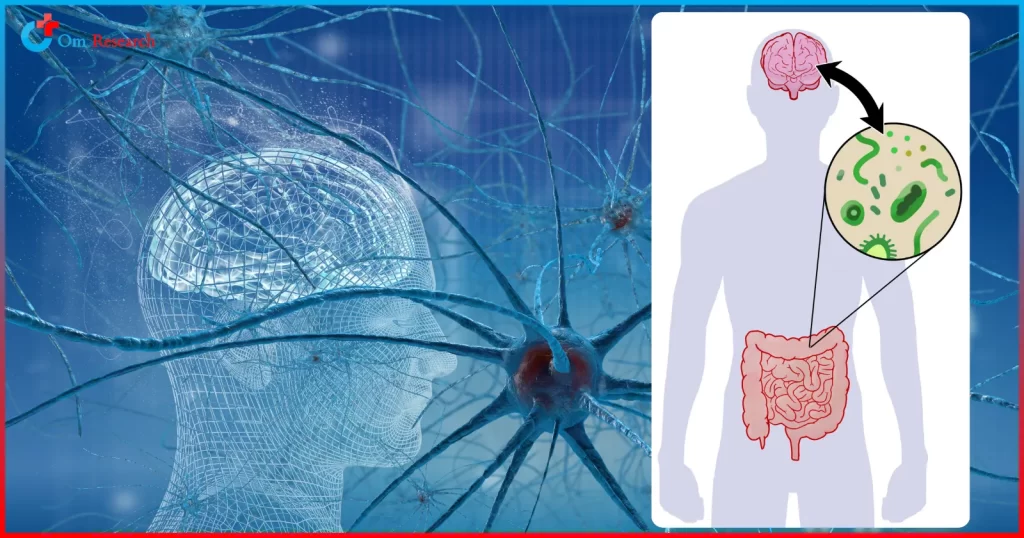
Understanding the Gut-Brain Axis
The gut and brain are in constant communication via the gut-brain axis, a bidirectional network involving nerves, hormones, and neurotransmitters. Think of it as a two-way highway: when stress activates the brain’s fight-or-flight response, it sends signals to the gut that can alter digestion, increase intestinal permeability, and even influence gut microbiota.
Conversely, an upset gut—whether due to inflammation, dysbiosis, or irritation—can send distress signals back to the brain, amplifying feelings of anxiety or fatigue.
For IBS patients, this axis is often hyperactive. Stress doesn’t just worsen symptoms like bloating, cramping, or irregular bowel movements, it can trigger them.
Studies show that individuals with IBS frequently report higher stress levels and are more likely to experience comorbid mental health conditions, including anxiety and depression.
How Stress Ignites IBS Symptoms
When stress enters the picture, several physiological changes occur:
- Hormonal Fluctuations: Cortisol, the body’s primary stress hormone, disrupts normal gut motility and increases visceral sensitivity, making even mild digestive activity feel painful.
- Neurotransmitter Imbalance: Stress depletes serotonin—a neurotransmitter produced largely in the gut—leading to altered bowel function and mood disturbances.
- Inflammation and Dysbiosis: Chronic stress weakens the gut barrier, allowing harmful bacteria to proliferate and triggering inflammatory responses that exacerbate IBS.
These mechanisms explain why a tense day at work might leave someone with IBS rushing to the bathroom or doubled over in pain. Over time, this stress-IBS cycle can become self-perpetuating, with physical symptoms causing additional emotional strain.
The Overlap with Mental Health
The link between IBS and conditions like Major Depressive Disorder (MDD) is profound. Research indicates that up to 60% of IBS patients meet criteria for a mental health disorder, with depression and anxiety being the most common. This isn’t coincidental: chronic pain, social stigma, and unpredictable symptoms can worsen quality of life, contributing to depressive episodes. Conversely, depression itself may heighten pain perception and disrupt gut function.
Strategies to Calm the Gut-Brain Axis
Managing stress isn’t just about feeling better mentally—it’s a critical step in managing IBS. Effective strategies include:
- Mind-Body Therapies: Cognitive Behavioral Therapy (CBT), mindfulness meditation, and yoga have been shown to reduce IBS symptom severity by calming the nervous system.
- Dietary Adjustments: Working with a dietitian to identify trigger foods (e.g., FODMAPs) while incorporating anti-inflammatory options like omega-3s and probiotics.
- Pharmacological Support: For some, low-dose antidepressants or gut-targeted medications can modulate nerve signals and reduce hypersensitivity.
The Role of Clinical Research in Advancing Care
For those seeking innovative solutions, clinical trials offer hope. Organizations like Om Research are actively investigating novel therapies targeting the gut-brain axis, including neuroactive probiotics, stress-resilience training programs, and medications designed to reduce visceral hypersensitivity. Participation in such trials not only contributes to scientific progress but may also provide access to cutting-edge treatments.
Final Thoughts
The gut-brain connection in IBS reminds us that health is deeply interconnected. By recognizing how stress shapes symptoms—and prioritizing both physical and emotional well-being—patients can reclaim control.
If you’re struggling with IBS, remember you’re not alone, and relief is possible. Whether through lifestyle changes, therapy, or clinical research,
Interested in learning more about how mental health intersects with IBS? Explore our blog on Major Depressive Disorder and its ties to chronic illness.
Om Research is committed to advancing treatments for conditions like IBS. Visit Enrolling Clinical Trials in California to discover ongoing studies and opportunities to participate.