Irritable Bowel Syndrome (IBS) is a complex gastrointestinal disorder characterized by abdominal pain, bloating, and altered bowel habits. While its exact cause remains elusive, research highlights that triggers play a pivotal role in flare-ups.
What Are IBS Triggers?
Triggers are external or internal factors that stimulate gut sensitivity in individuals with IBS. Unlike the root causes (e.g., gut-brain axis dysfunction or visceral hypersensitivity), triggers vary widely among patients. Identifying them requires a personalized approach, combining medical expertise with patient self-awareness.
Common Triggers of IBS
1. Dietary Factors
Diet remains the most frequently reported trigger. Specific food can irritate the gut lining, disrupt motility, or ferment in the intestines, leading to gas and bloating. Key food triggers include:
High-FODMAP Foods: Fermentable carbohydrates (e.g., onions, garlic, apples) draw water into the intestines and produce gas during fermentation. Studies show that a low-FODMAP diet alleviates symptoms in 70% of IBS patients
Dairy Products: Lactose intolerance mimics IBS symptoms, but even lactose-free dairy may trigger reactions due to milk protein sensitivity.
Caffeine and Alcohol: These stimulate intestinal contractions, often causing diarrhea or urgency.
Artificial Sweeteners: Sorbitol and mannitol, found in sugar-free products, act as osmotic laxatives.
Clinical Tip: Patients are advised to maintain a food-symptom diary to pinpoint dietary triggers.
2. Psychological Stress
The gut-brain axis links emotional stress to gastrointestinal function. Stress hormones like cortisol can:
- Increase intestinal permeability “leaky gut”.
- Alter gut motility, leading to spasms.
- Disrupt the balance of gut microbiota.
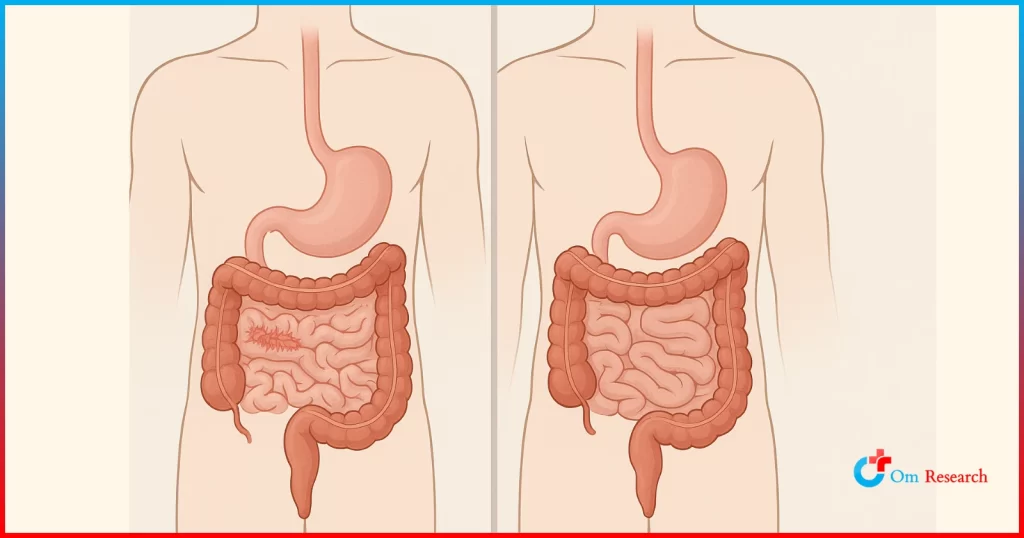
3. Gut Microbiome Imbalance
Dysbiosis, an imbalance in gut bacteria, is common in IBS patients. Antibiotics, infections, or diet low in fiber can deplete beneficial bacteria, heightening inflammation. Probiotics, particularly Bifidobacterium and Lactobacillus strains, have shown promise in restoring balance.
4. Hormonal Fluctuations
Women are twice as likely to develop IBS, and many report symptom exacerbation during menstruation. Estrogen and progesterone influence gut motility and pain perception, making hormonal shifts a key trigger.
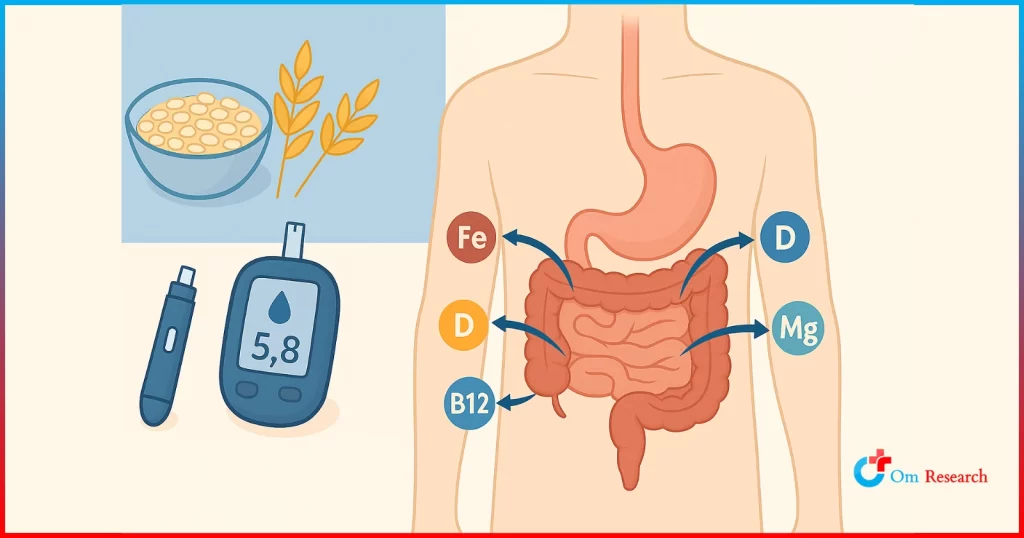
5. Medications
Antibiotics: Disrupt gut microbiota, increasing post-infection IBS risk.
NSAIDs (e.g., ibuprofen): Irritate the gastrointestinal lining.
Antidepressants: While some SSRIs help IBS, others may worsen constipation.
6. Sleep Disruption
Poor sleep quality disrupts the gut’s circadian rhythm, impairing its repair processes.
Om Clinical Research: Leading IBS Solutions
At Om Clinical Research, our clinical trials focus on:
Personalized Therapies: Testing gut microbiome-modulating treatments tailored to individual bacterial profiles.
Neuromodulation: Exploring non-invasive vagus nerve stimulation to calm gut-brain axis hyperactivity.
Dietary Innovations: Evaluating low-FODMAP and anti-inflammatory diets in diverse patient groups.
Participate in our IBS clinical trials to access cutting-edge treatments and contribute to groundbreaking medical discoveries.
Practical Steps for Managing Triggers
Adopt a Low-FODMAP Diet: Temporarily eliminate high-FODMAP foods, then reintroduce them systematically.
Prioritize Stress Management: Mindfulness, yoga, or therapy can mitigate gut-brain axis disruptions.
Stay Informed: Emerging research, such as Om Research’s clinical trials, continually refines our understanding of IBS.
Conclusion
Understanding IBS triggers empowers patients to move from frustration to control. While triggers vary, advances in clinical research are paving the way for personalized, effective treatments.
By participating in clinical trials, patients not only gain access to innovative therapies but also contribute to a future where IBS is no longer a chronic condition.