Clostridioides difficile (C. Difficile) infection is a severe gastrointestinal condition that leads to symptoms such as chronic diarrhea, abdominal cramps, and dehydration.
C. Diff. Colitis is often triggered by antibiotic use, which disrupts the intestine microbiome, allowing harmful bacteria to flourish.
While antibiotics are usually used to treat C. Diff. Colitis, many patients experience recurrent infections, causing a cycle of ineffective treatment.
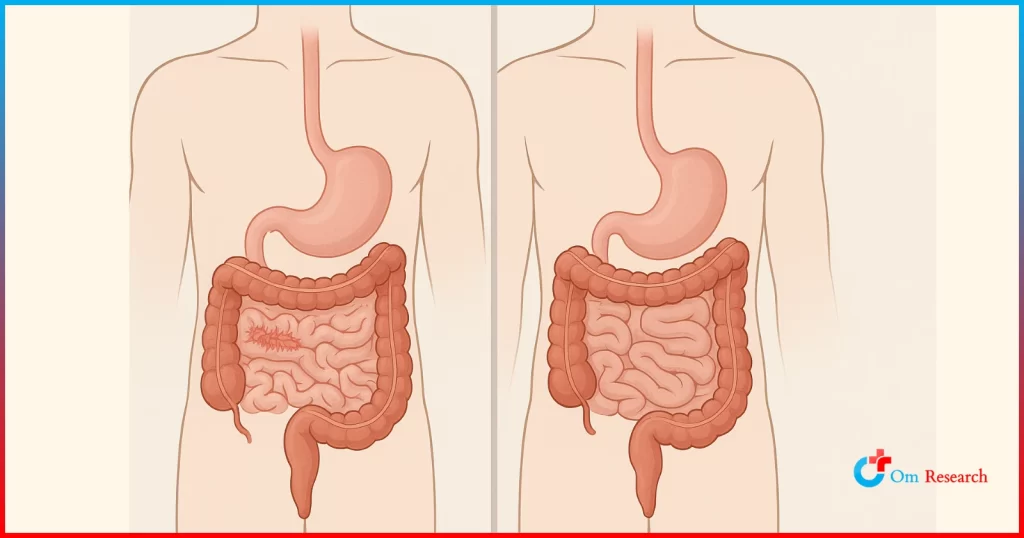
Fecal microbiota transplant (FMT) has emerged as a promising solution. The treatment involves transferring healthy intestinal bacteria from a donor to a recipient intestine to restore microbial balance and prevent recurrence.
With high success rates and growing clinical support, FMT has transformed the treatment approach for recurrent C. difficile infection.
What is Fecal Microbiota Transplantation (FMT)?
FMT is a medical procedure that cautiously restores the intestine microbiome by introducing healthy bacteria from the screening donor.
It restores good gut bacteria, increases variety, and lowers the risk of C. difficile overgrowth.
Traditional antibiotic remedies kill harmful and beneficial bacteria, often leading to microbiome imbalance.
On the other hand, FMT addresses the root cause by restoring direct microbial balance. This approach has demonstrated notable effectiveness, especially in cases where antibiotics fail.
Key Benefits of FMT:
- Helps break the cycle of recurrent C. difficile colitis.
- Restores microbial balance in the intestine.
- Reduces dependence on antibiotics.
- Improves overall intestinal health.
Clinical studies indicate recurrent C. Diff. Colitis in FMT. Treating Difficile infections has an efficacy rate of more than 85 percent, one of the most effective treatments available.
How is FMT Performed?
FMT involves transferring a processed stool from a healthy donor to the recipient through carefully controlled procedures to ensure safety and effectiveness.
FMT Process:
- Donor Screening: Potential donors must undergo extensive screening to ensure they are free from infection and harmful bacteria.
- Stool Processing: The collected samples are processed and filtered to separate beneficial microbes.
- Transplant: Microbiota is introduced into the patient’s intestine using one of the following methods:
Colonoscopy: The most common and effective approach is distributing the transplant directly into the large intestine.
Nasogastric/Nasoduodenal Tube: A tube is inserted through the nose in the stomach or small intestine.
Enema: A low-aggressive option but cannot be as effective as a colonoscopy.
Oral Capsules: Freeze-dried FMT capsules swallowed by the patient, eliminating the requirement of aggressive procedures.
FMT aims to safely restore the beneficial intestine bacteria, which improves the body’s natural capacity to fight infection.
Why FMT is Effective for Recurrent C. difficile Infections
The effectiveness of FMT comes from its ability to restore intestinal microbiota variety, which is often lost due to antibiotic use. Instead of eliminating bacteria, as antibiotics do, FMT introduces beneficial microbes, which compete with deficiency and prevent it from dominating the intestine.
Why FMT is more effective than antibiotics:
High Success Rate
- Studies suggest that FMT eliminates the recurrent C. Diff. Colitis in more than 85 percent of cases compared to 30–40 percent for antibiotics.
- Unlike antibiotics, which further interrupt microbiomes, the intestine restores its health, and FMT repair the intestines with healthy bacteria.
Reduces Antibiotic Resistance:
- The overweight of antibiotics contributes to drug-resistant bacteria. FMT provides a natural option that does not rely on antibiotics.
- Long-Term Security: Patients treated with FMT are significantly less likely to experience recurrent infections than those with antibiotic therapy.
Due to its success, FMT has been recognized as a viable treatment option and is being studied further for additional medical applications.
Future of FMT and Microbiome-Based Therapies
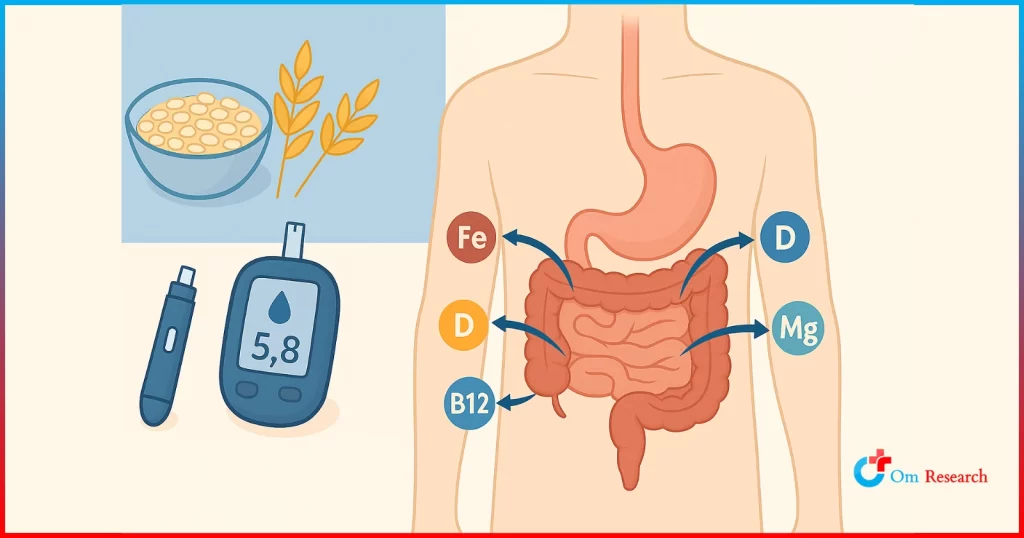
The success of FMT in treating C-difficile infections has increased interest in microbiome-based treatments for other conditions, such as:
- Irritable Bowel Syndrome (IBS): Possible relief for symptoms like inflammation and diarrhea
- Inflammatory Intestinal Disease (IBD): Possible benefits for Crohn’s disease and ulcerative colitis
- Metabolic Disorder: Research shows that gut bacteria are linked to conditions like obesity and diabetes.
- Autoimmune Status: Investigation is underway on how microbiome restoration can affect immune function
Progress in microbiome research
Researchers are developing synthetic microbiome-based treatments, which can serve as an alternative to traditional FMT in the future. It includes:
- Microbiome-Practical Drugs: targeted treatment designed to mimic the effects of FMT without the use of human stool
- Individual Probiotics: Bacterial formulation corresponding to specific diseases
- Advanced Stool Banking: Storage solution to preserve microbiota-rich samples for future use
Since the scientific understanding of the intestine microbiome has developed, microbiome-based treatments, including FMT, are expected to play a significant role in modern medicine.
By restoring the intestine microbiome, FMT effectively prevents the regrowth of harmful bacteria, improves intestinal health, and reduces the need for antibiotics.
With ongoing research on its application to other conditions, FMT represents a significant step in microbiome-based medicine.
As the understanding of intestine bacteria expands, treatments such as FMT can redefine treatment strategies for a wide range of gastrointestinal and metabolic disorders.
FMT is more than just an alternative treatment; This is a revolution in intestinal health restoration, providing a glimpse into the future of therapy.